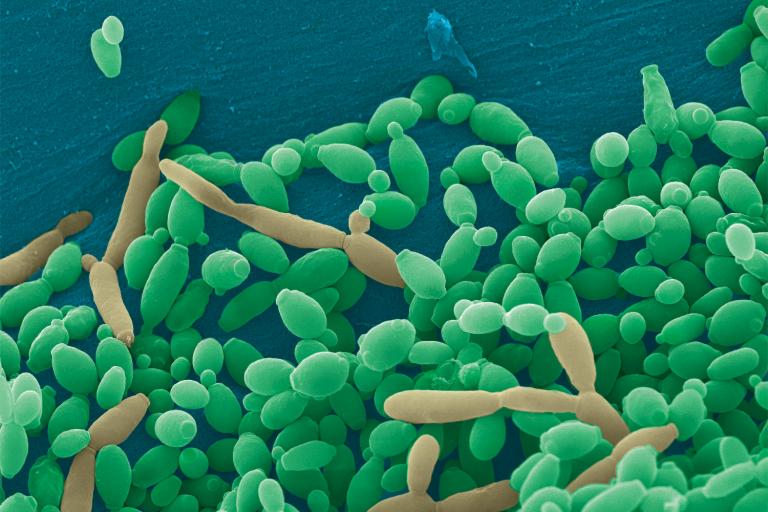
Fungi (yeast and mold) make up less than 1 percent of the microbes inhabiting your gut. Yet, scientists are finding that these fungi--your mycobiome--could have dramatic health effects.
If you've been struggling with digestive issues but can't find the culprit, balancing your gut mycobiome might be the missing link.
Fungi and Gut Bacteria
"It's important to consider both the bacteria and fungi in your microbiome because they interact with each other," says Mahmoud Ghannoum, PhD, author of Total Gut Balance ($27.95, Countryman Press, 2019) and director of the Center for Medical Mycology at Case Western Reserve University and University Hospitals Cleveland Medical Center.
For instance, if you take a broad-spectrum antibiotic for an infection, it can kill the bacteria in your gut, says Ghannoum. Without "good" bacteria to keep Candida albicans yeast in check, it can become invasive and cause oral, vaginal, or other infections.
The study of the fungi inside us is in its early days. Ghannoum coined the term "mycobiome" just a decade ago. New technology is aiding research in this area.
Risks of Gut Fungi Imbalance
Studies have found significant differences in the mycobiome of healthy people compared to people with various medical conditions.
These include, among others:
- obesity
- allergies
- digestive disorders
- autism
Sometimes it's uncertain whether a fungal imbalance is contributing to the medical condition or is a result of the condition.
Interaction with Crohn's Disease
In Crohn's disease, a type of inflammatory bowel disease, fungal imbalance seems to contribute to the condition.
Ghannoum and his colleagues found that people with Crohn's have a higher amount of Candida tropicalis in their gut. This yeast teams up with "bad" gut bacteria and forms biofilm (digestive plaque) to hide from your immune system and antimicrobial drugs.
The biofilm can damage and inflame your gut lining.
Small Intestinal Fungal Overgrowth
Candida is also commonly the culprit in small intestinal fungal overgrowth (SIFO). This can cause:
- chronic bloating
- indigestion
- belching
- nausea
- diarrhea
- gas
Testing Your Mycobiome
Some companies sell microbiome test kits directly to consumers. These mainly test for gut bacteria in your stool sample. Ghannoum developed a test at BIOHM Health (www.biohmhealth.com) that also looks at common fungi.
"We commonly see some level of Candida in the gut, even in healthy people," said Aubrey Phelps, MS, RDN, director of wellness at BIOHM Health. "We're looking to see if the Candida level is disproportionately high, which is when it's more likely to be problematic."
Common Intestinal Fungi
Phelps said some common fungi in stool tests include the following.
-
Candida
Prevalent strains include C. albicans and C. tropicalis
-
Pichia
This yeast may help keep Candida under control
-
Saccharomyces
A beneficial yeast; includes strains used to make fermented foods.
-
Aspergillus
This harmful mold contaminates some food, such as corn, and damp buildings.
Sources of Gut Fungi
"Initially, you get your mycobiome (such as Candida) from your mother," says Heather Hallen-Adams, PhD, a microbiologist and assistant professor at the University of Nebraska in Lincoln. "Later, you pick up fungi from your diet, the environment, and other people, such as by kissing. However, most fungi are just passing through and aren't really colonizing your gut."
For example, the DNA of mushrooms may be found in stool tests, but that doesn't mean the fungi are living in your gut. "Most edible mushrooms don't grow at human body temperatures--they generally prefer room temperature," says Hallen-Adams. "Penicillium mold used to make blue cheese doesn't grow at human body temperatures either."
The Saccharomyces cerevisiae yeast used to make bread can't colonize your gut. "Baking kills the yeast," says Hallen-Adams. "However, Saccharomyces could be alive in unfiltered beer, and Pichia is in some kombucha. So, these yeasts could show up in a stool test if you've consumed such beverages recently."
Balancing Your Gut Fungi
-
Healthy Diet
"Fungi and bacteria exist in your gut as part of a community," Phelps says. "You can nurture this ecosystem by eating a plant-based diet rich in fiber and getting plenty of anti-inflammatory omega-3 fats."
-
Probiotic Bacteria
Supplementing with probiotic bacteria, such as Lactobacillus acidophilus and Bifidobacterium breve, can be helpful.
These good bacteria inhibit Candida overgrowth and biofilm formation.
-
Enzyme Supplements
Preliminary studies suggest supplemental amylase, an enzyme, may inhibit the formation of biofilm.
-
Probiotic Yeast
Saccharomyces boulardii is the only yeast sold as a probiotic supplement. It interferes with Candida's ability to make biofilm.
S. boulardii may also alleviate diarrhea and other symptoms of irritable bowel syndrome.
-
Lifestyle
Do Don't Eat mostly whole, plant-based foods Eat highly processed and sugary foods Limit or avoid alcohol Drink alcohol routinely Exercise regularly Over-exercise without time for recovery Manage stress, such as with meditation Smoke Supplement with S. boulardii Take unnecessary antibiotics